Inside a coronavirus test lab
by Ailsa Harvey · 26/11/2020
Meet two scientists from the UK’s Covid-19 megalab, working around the clock to test the public
At the beginning of lockdown, virologist Ben and neuroscientist Beth were forced to stop all their practical work for their PhDs – but that wouldn’t keep them out of the labs. Because of their laboratory experience, the two scientists were asked to work on COVID-19 test samples, analysing swabs sent in by the public. During the months of April and May, Ben and Beth swapped their smaller Leeds-based labs for a newly built COVID-testing ‘megalab’ in Milton Keynes.
What made you want to work in these labs?
Beth: I was really missing being in the lab, and knew I had the skills to help. As soon as I got the email asking if I wanted to volunteer, I signed up. The process was fast after that and I got called up two days later.
Ben: I first heard about it through the Microbiology Society. An email was sent around because having experience in microbiology is helpful. I wasn’t doing much at the time and it was nice to feel like you were doing something helpful. It was exciting and new, and a whole different set up to what I’m used to.
Where did you work?
Beth: It was called the UK Biocentre in Milton Keynes. Before the pandemic they did other general diagnostic tests on patient tissue samples, but when the pandemic started they completely stopped that work and built this extra huge lab. Just a week before I started it was an empty building.
Ben: We stayed in a hotel nearby and went over to the lab for shifts. In the labs, it was very much a bubble system. You were allowed to stay with the 50 people on your shift. That was daunting because we had gone from socially distancing for about a month, to being around 50 people. In the hotel, we couldn’t really leave. You had to spend a lot of time by yourself.
What was the experience like for you personally?
Beth: It was probably one of the most intense experiences of my life. It was good to be there and I was really happy that I was helping, but by the end I had to leave. The atmosphere and other people working there made it a good experience. It kept me going knowing I was doing something worthwhile.
Ben: I really liked the sense of community. We were all there because we wanted to help. Although it was hard, it was nice that everyone was there wanting to do something good. When I started you had to sign up for a minimum of four weeks. Originally, I wanted to do it for the entirety of lockdown, until about August, but it was very intense and after one month I thought I couldn’t do it for much longer.
What did the training involve?
Beth: We were meant to have a few days of training on each step, but because we started during a final push towards reaching 100,000 tests a day, they were really trying to get it off the ground. We were chucked in the deep end and trained on the job. In the first few days we tried all the stages. After the training, people knew what they liked and the person in charge quickly identified which roles we were best at. I was quite fast at the first step and ended up staying there for ages.
Ben: First we had an induction day to get used to the environment and the setting. Then we would be trained in each stage of the process, with someone shadowing you and showing you how to do it. A lot of the jobs are very repetitive so there’s not so much of a learning curve. Over the course of a 12 hour shift you end up being pretty good at it.
How much pressure was there to meet a daily target?
Beth: I found that the pressure was more external, coming from the news and the government. The people at the testing centre had more of an attitude of ‘if you do it you do it’. They just wanted us to get as many tests done as we could. The tests coming into the lab came in peaks and troughs. At the beginning, there were so many tests coming in that it was quite overwhelming. Then, after they tested all the care homes it really slowed down for about two weeks. I think they were trying to decide who to test next. When they opened it up to anyone with symptoms it massively took off again. Watching the news, you could always predict whether you were going to have a quieter or busy shift- but there was always a lot to do.
Ben: Our boss was very results driven. That’s important for the situation we were in, but it was very much that you had the minimum break and often it was less than the minimum break. You would have to dash out, have a drink and come straight back. A 12-hour shift with no real break was very hard. There was a good atmosphere in the lab because we were steadily increasing our capacity and we were getting through more tests per day, but the government had put out an arbitrary target, which we didn’t reach.

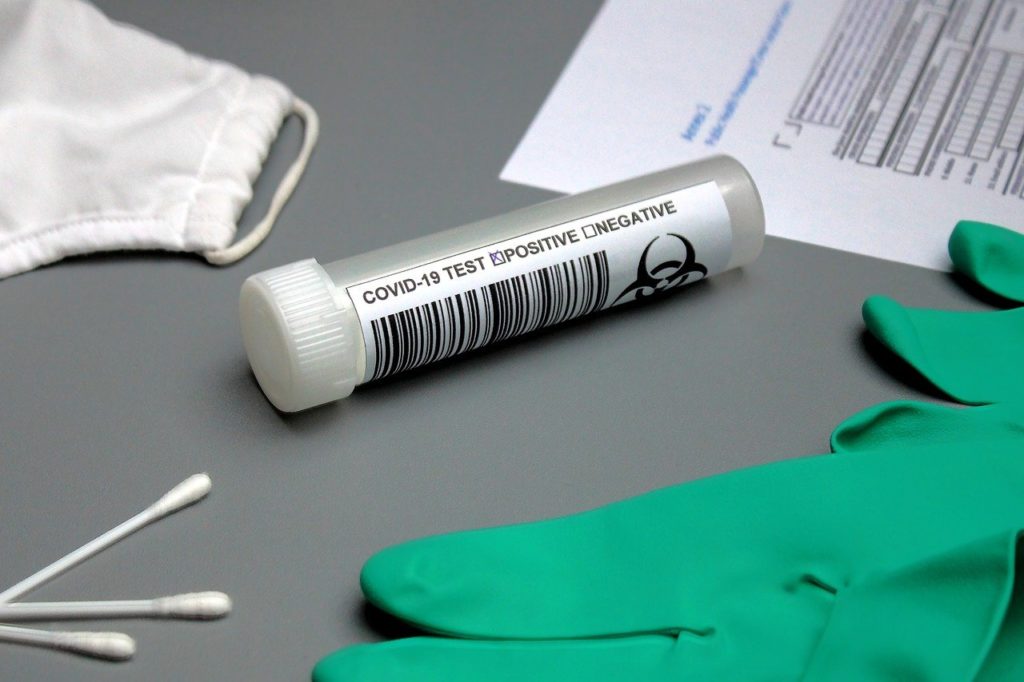
Samples can be dispensed by hand or robot (Image credit: RAEng_Publications)
How many tests did you usually process in a day?
Beth: When I was on the first step, inactivating the virus, I had 94 samples on each plate and it took between an hour and an hour and a half to do one plate. The most I ever did was around ten plates in a day. On my shifts we did around 20,000 tests. Milton Keynes was the biggest testing centre in the country, so our lab was a big chunk of the daily totals. The scientific process itself was quite fast, so I think the main delay in receiving results came from delivering the tests to the centre and then sending the results back.
Ben: Our boss would tell us every day how many we had completed in a shift. I think we did around 20,000 in 12 hours. They had a panel of results that told you how many were positive and negative.
What did your role involve?
Beth: We switched around different stages, but I spent a lot of time doing the first step, inactivating the virus. I opened the sample tube and put the contents on a testing plate. This step could either be done by hand or by robots. I didn’t really use the robots but by the time I left, they had doubled the number of robots to make things faster. While the robot was doing the work, you would always have to keep up with it and make sure all the lids were off for it and set up the tubes in place. You worked at the robot’s speed, so it was quite manic.
Ben: We spent a lot of time on one particular process, but we were able to do all of them as they needed to make sure if people left, or became ill, they could slot another person into that role and it wouldn’t slow down. Ideally, they wanted us to switch processes as a rest from repetitive jobs, but their priority was to keep the volume of tests going.
How accurate do you think the tests are?
Beth: As time goes on they will definitely be getting more and more accurate, but when I was there they were still finding their feet with how the test worked and what the good controls were to include. I don’t know the percentage error at the moment, but when I was there I think it was a 30 per cent error rate. That’s fairly high, but you have to remember that, in normal science, you do everything at least three times, whereas there you have one go at it. I do PCR tests a lot, and the threshold would usually be pretty high. But, in this circumstance it was low because they wanted to account for any detection of the virus. There are a lot of factors that can influence a test and I think when you do a test you should take it with a pinch of salt. You should definitely question a negative result if you know you have symptoms.
How different was this lab to the one you usually work in?
Beth: It was so different because we were told to turn off our science brains. You had to follow standard operating procedures really rigidly and there was no room for doing things your way. Even if you thought that there was a better way, you’d have to take it a lot higher up for that to be implemented. The main difference was that the implication of everything I did was a lot bigger. When I’m in the lab in Leeds, if I mess up it just gives me more hours of work, but in the COVID labs, that’s a person’s sample. Especially when it was whole care homes, you wanted it to be right. There’s only one sample for each person so you have to get it right the first time or that person has to do the test again, and I think it’s quite a traumatic test.
Ben: You were very much a cog in the wheel. You were part of a process that worked, so you didn’t have to improve it. Normally, in a research setting I’m often tweaking it. If I do a practical and something isn’t right, I can change it. That’s a big thing in science and I know a lot of people struggled with not being able to do that. We weren’t told much about the theory behind it and in a research setting that’s unheard of. Usually I know exactly how each technique works. If something goes wrong I can troubleshoot, whereas in this lab I was going in, pipetting and then leaving again. I quite enjoyed switching off and focusing on one technique. Obviously we were bothered about the final result, but that was someone else’s job. I just had to do my job and make sure it was done right.
Was there anything that surprised you about the lab?
Beth: There was no PPE a lot of the time when we were all together. We had to wear PPE when we were handling the virus samples, but because we had to work really close together there was less focus on socially distancing with each other. I was surprised with how little thinking I was required to do. I remember thinking ‘what if I don’t know enough?’ and ‘what if I’m completely out of my depth?’ but we just had to use manpower. I had also never seen such a big scale operation, because I had always worked in really tiny labs.
Ben: The application said that you would need a lot of experience, but I met one person who started who was a college student and she didn’t even know how to pipette. That’s no insult to her because I didn’t know how to pipette when I was a college student, but you don’t expect a college student to be in a diagnostic laboratory working on the Coronavirus. It was quite startling. I think that was a rarity though, and I like to think that when they started hiring people full-time they had a more thorough interview process.
Are you glad you volunteered?
Beth: I’m really happy I did it and the whole experience was really eye opening. I worked with scientists of all backgrounds and of all ages and there was no hierarchy. So that was a really unique experience that I will never really get again.
Ben: I’m definitely glad I did it and it was different to anything I have experienced. I think I’ve grown a lot as a person doing it and know how much I can push myself. It was really stressful at the time, but looking back it’s nice to know that I helped out during this pandemic. If I hadn’t applied for it I would have regretted it for the rest of my life.
For more science and technology articles, pick up the latest copy of How It Works from all good retailers or from our website now. If you have a tablet or smartphone, you can also download the digital version onto your iOS or Android device. To make sure you never miss an issue of How It Works magazine, subscribe today!